TRICARE does occasionally cover TMS therapy, but only in certain circumstances. Anyone who is depressed might be wondering, “Does TRICARE pay for TMS therapy?” The answer is yes, but only if certain conditions are met.
Currently serving in or having served in the military can be very hard. Some veterans and active-duty military members have special mental health problems, like anxiety, depression, and PTSD.
Watching someone you care about struggle with these problems is hard, especially when standard treatments don’t seem to help.
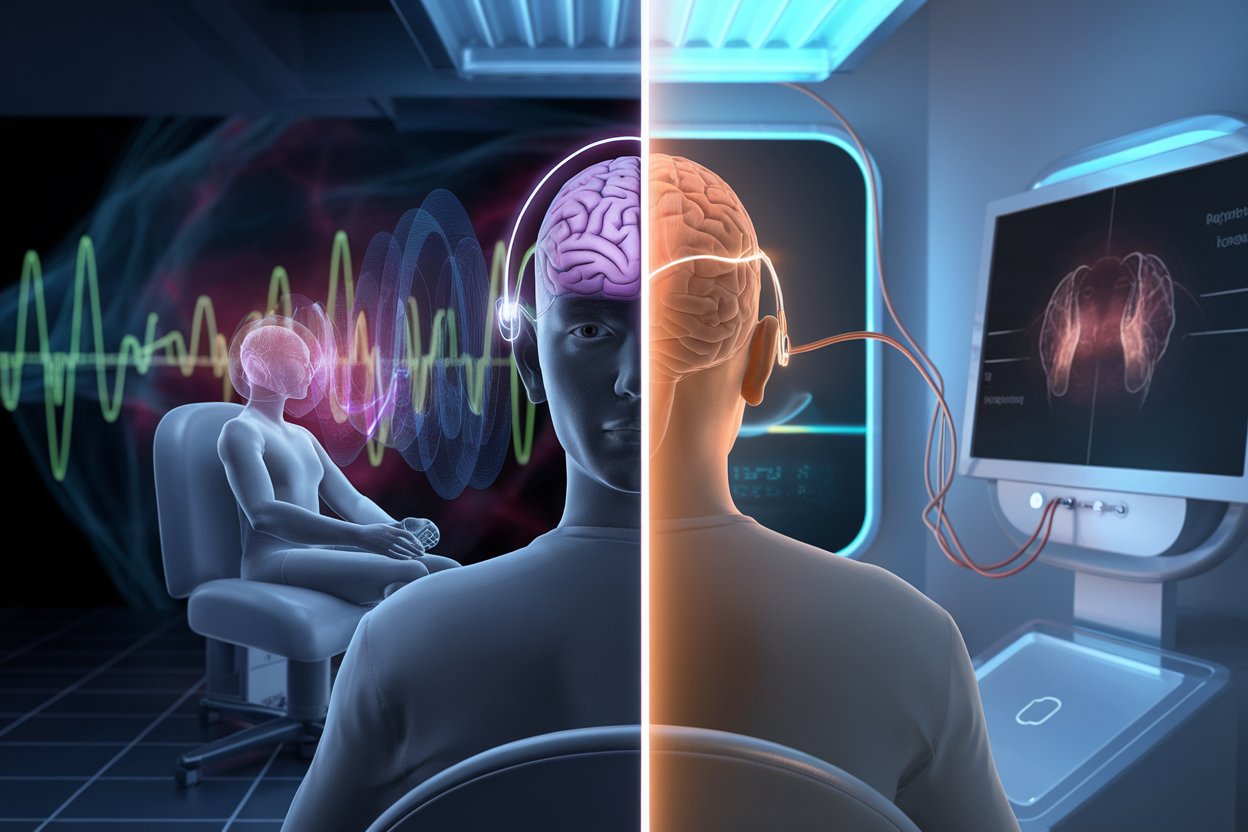
To help people with depression, transcranial magnetic stimulation (TMS) uses magnetic fields to help their symptoms. The benefits of TRICARE and TMS therapy will be discussed.
What is TMS Therapy and What Does it Do?
Magnetic fields are used in TMS to stimulate nerve cells in the brain without hurting the person. This stimulation might help people who are depressed feel better.
TMS is especially helpful because it can be done without anaesthesia, doesn’t require hospitalisation, and has fewer side effects than regular antidepressants. TMS works very well for people who haven’t responded well to other treatments.
What Disorders Does TRICARE Cover for TMS?
TRICARE is a health insurance plan for people in the military, veterans, and their families. If medication, therapy, and other treatments for Major Depressive Disorder (MDD) have not helped, TRICARE will pay for TMS therapy. MDD is a very bad form of depression that makes it hard to do normal things.
Conditions Not Covered:
TRICARE does not yet cover them for TMS therapy, even though some scientific studies have shown that TMS and rTMS may help treat these conditions.
Connections Between PTSD, Concussions, and MDD
Veterans and people who are still in the military often have problems with PTSD and concussions. On occasion, these health problems can cause or make MDD worse. People who suffer from depression can find hope in TMS therapy, which has been shown to help heal MDD. For now, TRICARE does not cover TMS therapy for PTSD, anxiety, or concussion symptoms.
However, it is important to keep in mind that these conditions often happen along with MDD. It’s even more important for mental health in general to deal with MDD than before.
As shown in a study by Janicak et al. (2008), TMS therapy can help treat MDD. Patients who had not responded to other treatments showed significant improvement. There is a lot of overlap between MDD, PTSD, and concussions, which makes it harder for military members and veterans to live a normal life.
Symptoms TMS Has Been Shown to Address
Besides MDD, TMS therapy has shown promise in addressing symptoms like:
- Anxiety (not yet covered by TRICARE)
- PTSD symptoms (not yet covered by TRICARE)
- Headaches from concussions (not yet covered by TRICARE)
Although they are not on the label and have not received FDA approval, these advantages are the result of scientific studies. For TRICARE to cover these conditions, more research needs to be done.
Why TRICARE holders frequently seek out TMS
TMS therapy is often sought after by people with TRICARE because it is a non-invasive way to treat MDD without using medication. A lot of active-duty military and veterans have tried many medicines and treatments that didn’t work.
For people who haven’t gotten better with other treatments, TMS gives them new hope. It works well to treat MDD, which makes it a good choice for people with depression when other treatments haven’t helped.
FDA Approval and TRICARE Coverage
The FDA has approved TMS therapy as a way to treat MDD. TRICARE will only pay for TMS if the patient has already tried other treatments that didn’t work. This means that traditional therapy and medicines must not have worked before TRICARE will pay for TMS.
Are You or a Loved One Struggling?
Call us at (602) 922-0284
Do you qualify for a free EEG and psychiatric evaluation? Contact American TMS Clinics in Phoenix, Arizona, today to find out!
American TMS Clinics is a fully accredited TRICARE TMS provider in Phoenix Arizona, dedicated to helping you on your journey to better mental health.
CONTACT AMERICAN TMS CLINICS TODAY
FAQs About TMS Therapy and TRICARE Insurance
Is TMS covered by TRICARE insurance?
Yes, TRICARE covers Transcranial Magnetic Stimulation (TMS) therapy, but only under specific conditions. TRICARE covers TMS for treating Major Depressive Disorder (MDD) when other treatments, such as medication and traditional therapy, have not been successful.
What does TMS therapy cost?
The cost of TMS therapy can vary widely depending on the provider and the number of sessions required. On average, a full course of TMS therapy can cost between $6,000 and $12,000. However, if you have TRICARE and meet the necessary requirements, this cost can be significantly reduced or fully covered by your insurance.
What qualifies you for TMS?
To qualify for TMS therapy, you generally need a diagnosis of Major Depressive Disorder (MDD) and must have tried and failed to respond to other treatments, such as antidepressant medications and traditional therapy. Your healthcare provider will evaluate your medical history and current condition to determine if TMS is a suitable option for you.
How long does it take insurance to approve TMS therapy?
The approval time for TMS therapy can vary depending on your insurance provider and your specific situation. With TRICARE, the process usually involves your healthcare provider submitting a request along with your medical records and a treatment plan. Once submitted, it can take a few weeks for TRICARE to review and approve the request. It’s essential to stay in communication with your provider and TRICARE to ensure all necessary documentation is submitted promptly.
How do you qualify for TMS with TRICARE?
To qualify for TMS therapy with TRICARE, you need to have a diagnosis of Major Depressive Disorder (MDD) and must have tried other treatments without success. This means you should have undergone medication and traditional therapy, but did not achieve the desired improvement. Your healthcare provider will need to provide documentation of your treatment history and current condition to TRICARE as part of the approval process.
What will TRICARE not pay for?
TRICARE does not currently cover TMS therapy for conditions other than Major Depressive Disorder (MDD) and Obsessive Compulsive Disorder (OCD). This includes:
-
- Anxiety disorders
-
- Bipolar disorder
-
- Post-Traumatic Stress Disorder (PTSD)
-
- Concussions
Even though TMS has shown promise in treating these conditions in some scientific studies, TRICARE only covers TMS therapy for MDD at this time.
Sources:
-
- Health Net Federal Services. (2021). “Transcranial Magnetic Stimulation (TMS) for Depression.”