Transcranial Magnetic Stimulation (TMS) is a new concept in the field of mental health treatment that shows promise for people with depression and Obsessive-Compulsive Disorder (OCD).
By using the power of magnetic fields, TMS gives patients who haven’t had much success with other treatments a way to get better that doesn’t involve surgery or drugs. This study goes into detail about the interesting science behind TMS and shows how this new treatment is changing people’s lives.
Understanding TMS and Its Origins
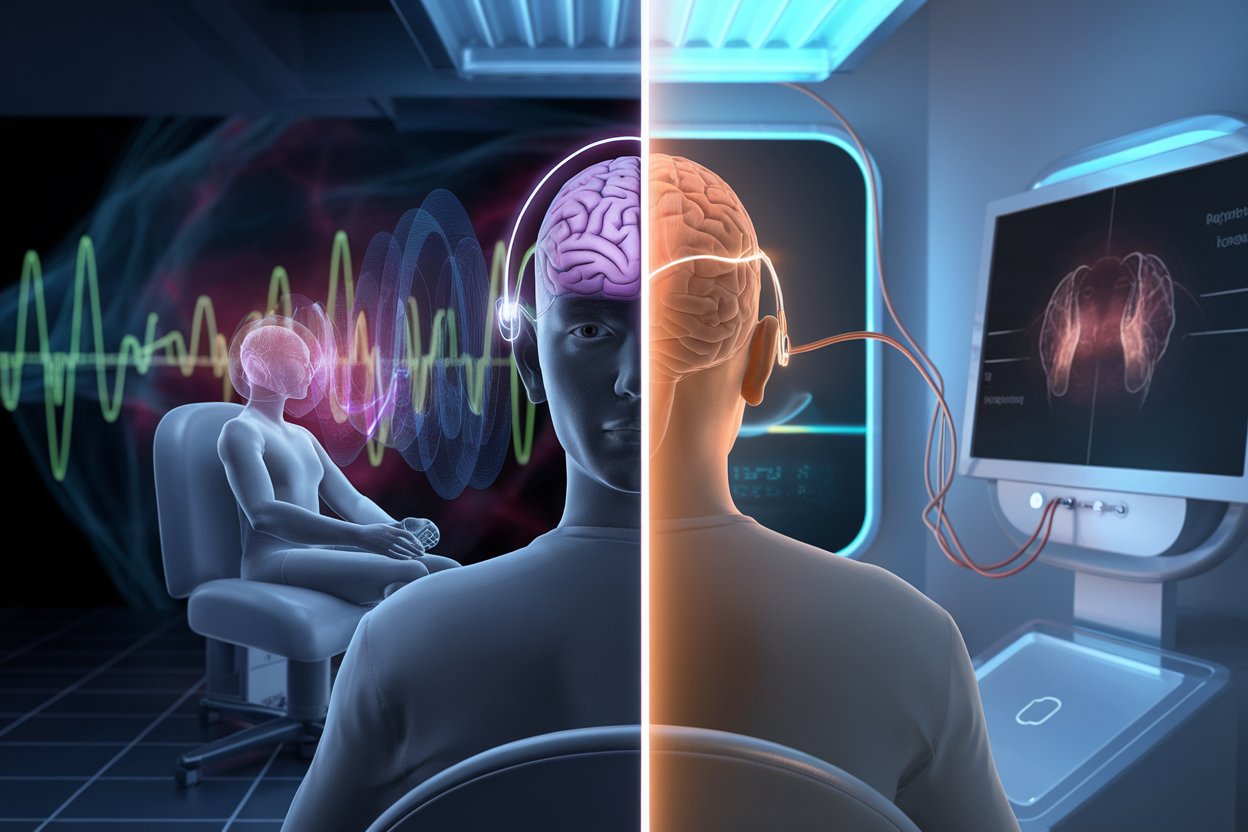
Transcranial Magnetic Stimulation is a new way to treat mental illness that uses magnetic fields to stimulate nerve cells in the brain, focusing on areas that control depression and mood. TMS was created in 1985 and has been through a lot of research and clinical trials to prove that it works. Its non-invasive nature makes it stand out, giving people who are looking for solutions other than traditional drug treatments a choice.
TMS went from being an experimental method to an FDA-approved treatment for depression in 2008 and then for OCD in 2018. This shows how far we’ve come in understanding and treating mental health problems. By changing neural activity, TMS helps us understand how flexible and able to change the brain is, which opens the door to new treatments.
How TMS Treats Depression: The Mechanism Explained
Targeted magnetic pulses are used in TMS therapy for depression to reset and rebalance the brain’s electrical impulses. This is based on the idea of neuroplasticity. It is thought that this process turns on parts of the brain that aren’t working as well in people with depression, which makes them feel better and lessens their symptoms.
Because TMS is so precise, it can be used to give a focused treatment that is tailored to each person’s neuronal architecture, making it a more personalized way to recover.
Clinical studies have shown that TMS-induced changes in neuronal activity significantly improve depressive symptoms, frequently when other treatments have failed. This has big implications for how depression will be treated in the future because it gives people who don’t respond to antidepressants another good option.
TMS for OCD: A New Horizon in Treatment
Exploring how TMS can be used to treat OCD is an exciting new area of psychiatry. While the main goal of treatment for depression is usually to improve the person’s mood, TMS for OCD focuses on the complex brain circuitry that controls the obsessive thoughts and behaviors. By focusing on the parts of the brain that are linked to these compulsions, TMS helps to lessen their intensity and frequency, giving relief to people who suffer from them.
The Treatment Process: What to Expect from TMS
The first step in TMS treatment is a full evaluation so that the therapy can be tailored to each person’s needs. For 30 to 60 minutes at a time, a magnetic coil is placed near the head during sessions.
Patients may feel like they are being tapped while magnetic pulses are being applied, but the procedure is usually not painful. Five days a week sessions are suggested for four to six weeks. Many patients say their symptoms get better as early as two weeks into treatment.
More clinics around the world now offer TMS therapy, making it easier for more people to get it. Even though the thought of going to sessions every day might be scary, TMS’s non-invasive nature and high success rate make it a good choice for many. Patients often go back to their normal lives right away after treatment, with few to no side effects.
Success Stories: Real-life Impacts of TMS on Mental Health
The people whose lives TMS has changed are the true witnesses to its effectiveness, not the statistics and clinical trials. TMS has brought hope back to people who had lost it, like veterans with PTSD and moms with postpartum depression. One interesting story is about a young artist with severe OCD who got a new lease on life after a series of TMS sessions. Without the restrictions of his compulsions, he was able to return to his art and passions.
Navigating the Challenges of TMS Therapy
TMS has some good results, but it’s not a solution that works for everyone. One of the biggest problems patients have is that their insurance doesn’t always cover TMS. Also, going to treatment every day for a few weeks can be hard for some people to make time for. Clinicians are actively working to get around these problems by pushing for more insurance coverage and researching protocols that might allow for fewer sessions without lowering the effectiveness.
The Future of TMS in Mental Health Treatment
The future for TMS in mental health care is big and bright. More research and technological advances are being made to make it more accurate and useful for a wider range of psychiatric disorders besides OCD and depression. As we learn more, TMS might be able to work with other types of therapy, like cognitive behavioral therapy and medication. This could lead to even more effective, all-around treatment plans that are tailored to each person’s specific needs.
Embracing the Future of Mental Health Treatment
More research is needed to fully understand mental health issues. The development of TMS from a theory to clinical use shows a promising new way to treat mental illnesses. Its ability to target specific parts of the brain that control mood and compulsive behaviors offers a personalized approach that is both new and hopeful.
TMS for mental health is more than just a treatment for people with depression and OCD. It’s a chance for a fresh start and a reminder of the need to keep looking for solutions that respect the mind’s complexity and the person’s path to wellness.