Transcranial Magnetic Stimulation (TMS) is a revolutionary treatment method for those struggling with depression, especially when other therapies have failed. As someone who’s been exploring options for mental health treatments, you may have heard about TMS.
But how safe is it? That’s a big question! Let’s take a closer look at what TMS is, its safety, and what you need to know before you start treatment.
Introduction to TMS and Its Importance
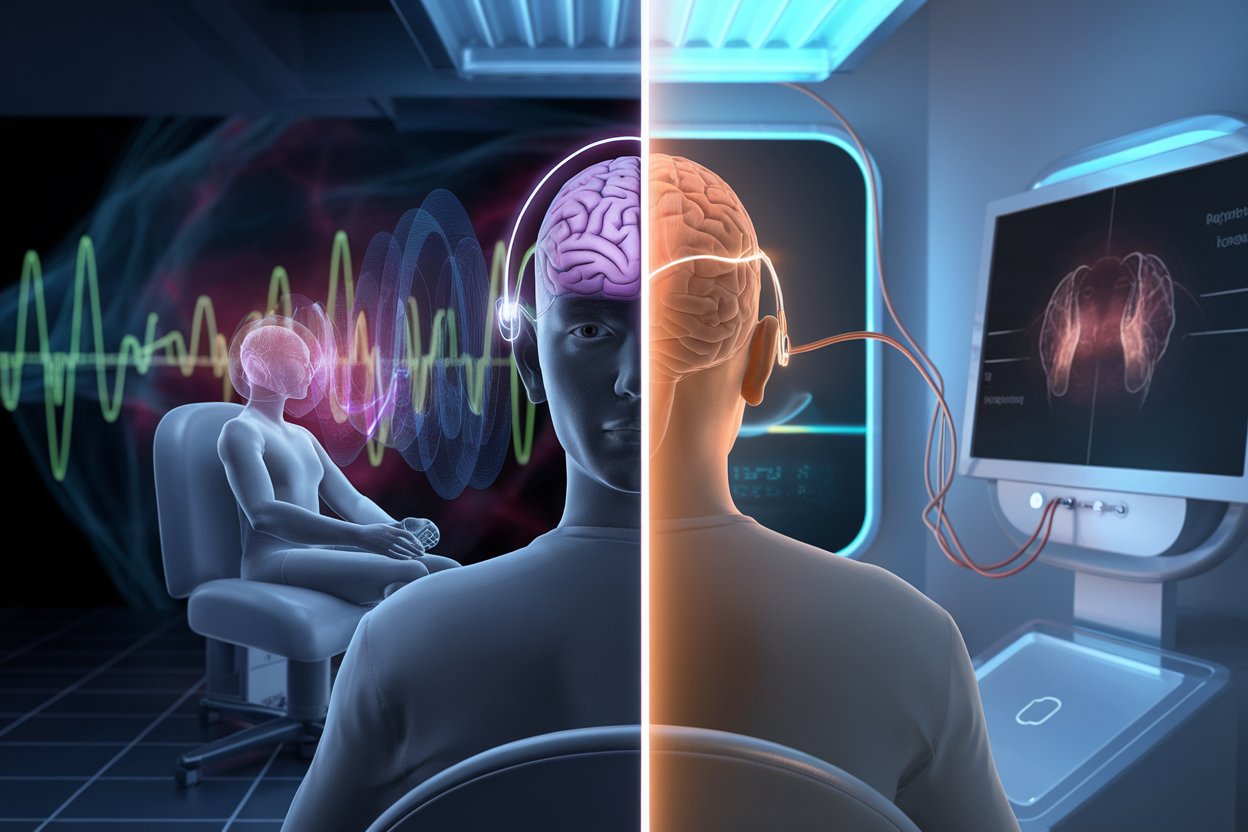
TMS, or Transcranial Magnetic Stimulation, is a non-invasive treatment designed to treat depression by using magnetic fields to stimulate nerve cells in the brain. Unlike traditional treatments that may involve medication or even surgery, TMS is a safe and non-invasive option that helps restore brain function.
The primary reason why TMS is important is that it offers a glimmer of hope for individuals who haven’t found relief from medications or other therapies. This non-surgical method is a breakthrough for those struggling to combat depression and can provide a lifeline when other treatments have failed.
What makes TMS especially appealing is its ability to target specific areas in the brain responsible for mood regulation. It’s like giving your brain a gentle push to help it work better.
The best part? No surgery and no heavy medication. However, before diving into treatment, it’s crucial to understand the risks and benefits associated with TMS safety.
Understanding TMS Safety: An Overview
When you’re considering TMS treatment, it’s natural to wonder about the safety of the procedure. The short answer is that TMS is generally considered safe for most people.
The treatment uses magnetic fields to stimulate nerve cells in areas of the brain that control mood and emotion. While TMS side effects are typically mild, such as headaches or mild discomfort at the treatment site, they are temporary and usually dissipate after a few sessions.
However, as with any medical treatment, TMS does come with some risks. Serious side effects are extremely rare but may include seizures. For this reason, it’s essential to have a comprehensive discussion with your doctor before starting treatment.
Your healthcare provider will review your medical history and evaluate whether TMS is the right treatment option for you, based on your individual health status.
Key Considerations Before Starting TMS Treatment
Before beginning TMS therapy, there are several important things to consider. This is a non-invasive treatment that requires your commitment over several weeks, so it’s essential to fully understand what to expect.
While TMS offers hope for those struggling with depression, it’s not a quick fix, and certain factors must be evaluated beforehand. Here’s what you need to know:
1. Treatment Duration and Commitment
- TMS therapy requires multiple sessions, typically 4-6 weeks, with each session lasting around 20-40 minutes.
- It’s important to stay committed to the treatment schedule for the best results.
- Expect gradual improvements as the brain begins responding to the stimulation.
- Consistency is key; skipping sessions can delay or reduce the effectiveness of treatment.
2. Side Effects and Risks
- Most people experience mild side effects like headaches, scalp discomfort, or lightheadedness.
- These side effects tend to subside after a few sessions and are not usually long-lasting.
- Serious side effects, such as seizures, are rare but possible, so a thorough evaluation is required.
- Hearing protection is often used during the procedure to prevent hearing damage from the machine’s noise.
3. Insurance and Financial Considerations
- TMS treatment is not always covered by insurance, so it’s crucial to check with your provider before starting.
- Some insurance plans may require prior authorization or specific criteria for approval.
- If insurance coverage is not available, the cost of treatment can be significant, so consider your financial readiness.
- Some TMS clinics offer financing options or sliding scale fees, so inquire about available options.
Common Side Effects and Risks of TMS
As with any treatment, TMS comes with its own set of risks. Fortunately, most side effects are mild and temporary. The most common side effects are headaches or discomfort at the site where the magnetic pulses are administered. Some people also report feeling lightheaded or fatigued during or after their sessions. These side effects are usually short-lived and diminish with continued treatment.
Serious side effects, such as seizures, are extremely rare but are still a possibility. Although the risk is low, it’s important to be aware of this potential issue. Additionally, hearing loss can occur due to the loud clicking sounds produced during the procedure. However, this risk is typically managed with earplugs, which are provided to patients before treatment.
Mood changes may also occur, especially in individuals with underlying anxiety or depression. These fluctuations are normal but should be monitored. It’s always best to communicate openly with your healthcare provider to ensure your treatment plan remains safe and effective.
How to Assess if You’re a Good Candidate for TMS
Not everyone is a good candidate for TMS therapy, and understanding if it’s the right treatment for you is crucial. TMS is primarily used to treat depression, particularly in individuals who have not responded to traditional treatments like medication or therapy. If you’ve tried various treatments without success, TMS could be a viable next step.
However, if you have metal implants in or near your head, such as a pacemaker, cochlear implants, or certain dental devices, TMS may not be suitable for you due to the risks associated with the magnetic pulses. Additionally, if you have a history of seizures, TMS may also pose a risk. Your doctor will thoroughly assess your medical history to determine if TMS is safe and appropriate for your specific condition.
Pre-Treatment Evaluations for Ensuring TMS Safety
Before undergoing TMS treatment, you will likely undergo a pre-treatment evaluation to ensure it’s safe for you. This evaluation includes a thorough review of your medical history, including any mental health conditions, past treatments, and overall health. Your doctor will also ask about any medical devices or metal implants in your body, as these can affect the safety of TMS.
This evaluation is crucial to ensure TMS safety, as it helps to identify potential risks and ensures that the treatment is tailored to your specific needs. If your doctor deems TMS suitable for you, they will create a personalized treatment plan that aligns with your health profile.
Tips for Choosing a Reputable TMS Provider
Choosing a reputable TMS provider is essential for a safe and effective treatment experience. When researching providers, look for one that has a track record of success and is licensed to perform TMS. Ask about their experience with treating patients, the number of successful treatments they’ve administered, and their patient outcomes.
It’s also important to check for patient reviews. Positive feedback and testimonials can give you insight into the provider’s quality of care. During your initial consultation, ask questions about their approach to treatment and their commitment to patient safety. A good provider will always be transparent about their qualifications and willing to answer all your questions.
What to Expect During a TMS Session: Safety Procedures
When you arrive for your TMS session, you’ll be seated comfortably in a chair, and a magnetic coil will be placed near your head. The coil will deliver brief magnetic pulses to stimulate the areas of your brain that regulate mood. You will remain awake during the procedure, and the treatment itself typically lasts 20 to 40 minutes per session.
Safety procedures are in place to ensure your comfort and well-being during the session. For instance, earplugs will be provided to protect your hearing from the loud clicking sounds produced by the magnetic pulses. The technician will adjust the machine and the coil to ensure that the pulses target the correct area of your brain.
You’ll also have the opportunity to communicate with the technician throughout the session to ensure your comfort.
Aftercare and Monitoring for TMS Safety
After your TMS session, your provider will monitor your progress to ensure the treatment is working as expected. Most people experience mild side effects like headaches or scalp discomfort, but these usually go away after a few sessions. If you experience persistent or severe side effects, it’s important to contact your provider immediately.
During follow-up visits, your doctor will evaluate your progress and make any necessary adjustments to your treatment plan. Monitoring after treatment is an essential part of the process, as it ensures the treatment remains safe and effective.
Conclusion: Making an Informed Decision on TMS
Making an informed decision about TMS treatment is essential for your mental health journey. While TMS has proven to be a safe and effective option for many individuals suffering from depression, it’s important to consider the potential risks and side effects. By consulting with your doctor and carefully weighing the pros and cons, you can determine if TMS is the right choice for you.
Remember, your mental health matters, and with the right information, you can make an empowered decision that will help you feel better and take control of your mental health.
For more information on TMS and to find a certified provider near you, visit American Psychiatric Association.