If you’re considering Transcranial Magnetic Stimulation (TMS) therapy, you’re probably asking, “Will insurance cover TMS therapy?” The cost of TMS can be significant, so understanding if your insurance will cover it is crucial. Let’s explore how insurance coverage for TMS therapy works, who qualifies, and what you need to know to improve your chances of getting coverage.
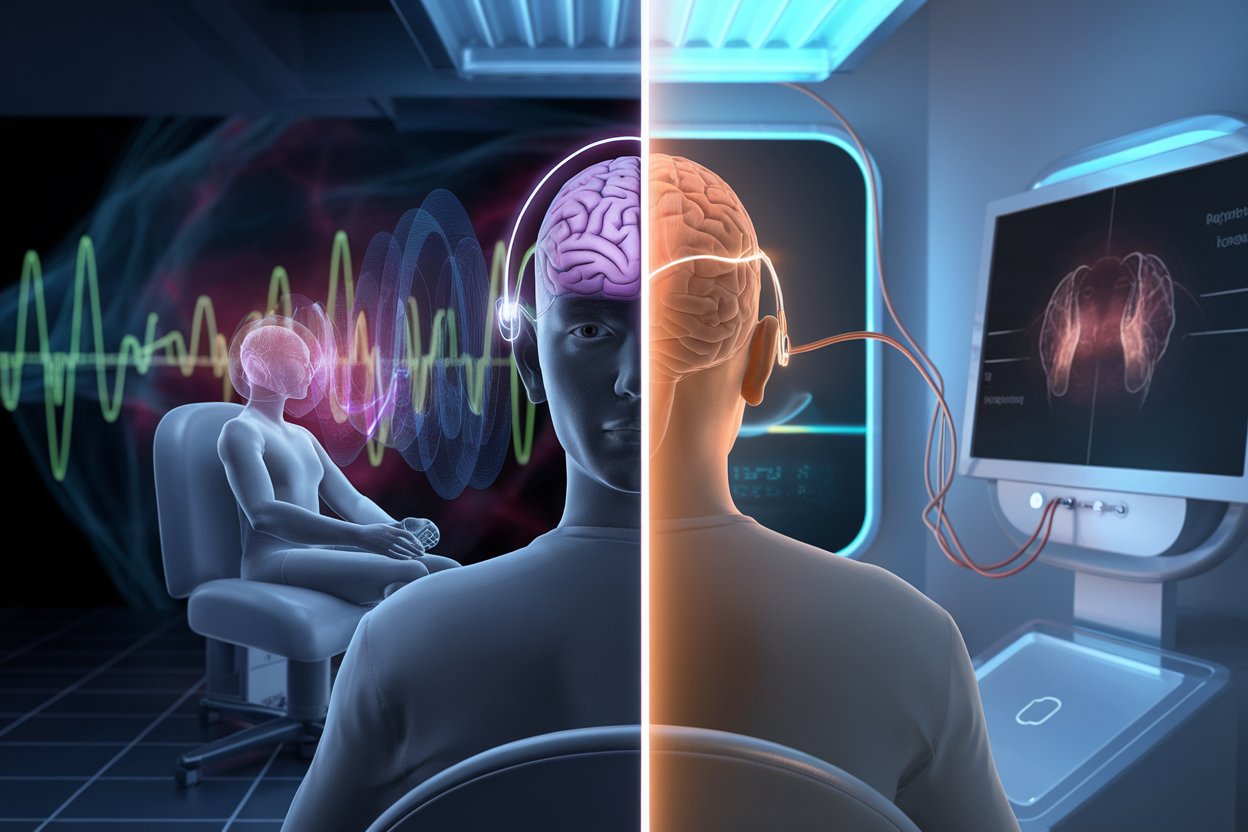
What is TMS Therapy?
TMS therapy is a noninvasive procedure that uses magnetic pulses to stimulate certain parts of the brain. It’s most often used for treating major depressive disorder (MDD) when other treatments like medications and therapy haven’t worked. TMS is typically recommended for those with treatment-resistant depression.
The treatment involves sitting in a chair while a magnetic coil is placed on your head. This coil sends magnetic pulses to target areas of the brain. Sessions last around 30 to 60 minutes, and a full treatment course usually requires multiple sessions over several weeks.
Will Insurance Cover TMS Therapy?
Will insurance cover TMS therapy? This is one of the most common questions patients ask. The answer depends on your insurance provider, your specific plan, and whether you meet certain criteria. Many major insurance companies do cover TMS therapy, but there are specific requirements you must meet to qualify.
Requirements for TMS Therapy Coverage
Most insurance providers consider TMS therapy medically necessary only for patients with specific conditions. Typically, TMS is covered for people with moderate to severe major depressive disorder who have:
- Tried at least two antidepressant medications without success.
- Completed talk therapy without sufficient improvement.
- A diagnosis is provided by a licensed mental health professional.
These requirements vary among different insurance companies, so it’s essential to check with your insurer directly to know their specific criteria.
TMS Therapy Cost with Insurance Coverage
If your insurance plan covers TMS therapy, you may still have out-of-pocket costs. This can include co-pays or coinsurance, which range from $10 to $70 per session depending on your plan. A complete TMS treatment often requires about 36 sessions, so it’s helpful to know these costs ahead of time.
Insurance coverage typically includes a brain mapping session, which is done before treatment begins to identify the optimal areas of the brain to target.
TMS Therapy Cost Without Insurance Coverage
Without insurance, TMS therapy can be quite costly. A single session can range from $400 to $500, and a full course of treatment could cost around $15,000. Many clinics offer payment plans or financing options, so you may still be able to receive treatment even if your insurance does not cover it.
What Insurance Providers Cover TMS Therapy?
Will insurance cover TMS therapy? Yes, many major insurance providers do. These include:
- Aetna
- Blue Cross Blue Shield
- Cigna
- United Healthcare
- Medicare
- Tricare
However, each provider may have specific requirements. For example, Blue Cross Blue Shield typically requires that you’ve tried at least two antidepressants before they approve coverage for TMS.
How to Improve Your Chances of TMS Coverage
If you want insurance to cover TMS therapy, you need to meet certain criteria and provide documentation. Here are some tips to improve your chances:
- Document Previous Treatments: Make sure you have detailed records of the antidepressants and therapy you’ve tried. Insurers will want proof that other treatments didn’t work.
- Get a Letter from Your Doctor: A letter from your mental health professional stating that you have a major depressive disorder and that other treatments have failed can help.
- Follow Your Treatment Plan: Insurance companies may deny coverage if they see missed therapy appointments or medication doses. Following your prescribed treatment plan can demonstrate that you’re serious about your care.
Potential Disqualifications for TMS Coverage
Not everyone qualifies for TMS therapy coverage. Here are some common reasons why insurance companies may deny coverage:
- Pregnancy or Nursing: There is limited research on the safety of TMS during pregnancy.
- History of Seizures: If you have a history of seizures or certain neurological conditions, insurers might not cover TMS due to the risk involved.
- Presence of Metal Implants: People with metal implants near their head, such as cochlear implants or aneurysm clips, may not be eligible.
What to Do If TMS Therapy Coverage Is Denied
If your insurance company denies coverage for TMS therapy, don’t lose hope. Here are a few steps you can take:
- Appeal the Decision: Many insurance providers have an appeals process. Work with your doctor to submit additional documentation and try to appeal the denial.
- Seek Financial Assistance: Some clinics offer sliding-scale payment options based on your income. There are also medical financing programs that can help make TMS more affordable.
- Consult with Your Provider: Ask your mental health professional for advice. They might have experience working with your insurance company and can help provide additional information to strengthen your case.
Is TMS Covered by Medicare and Medicaid?
Medicare and Medicaid do cover TMS therapy, but the requirements are similar to private insurance. You must have a diagnosis of major depressive disorder and show that other treatments have failed. Medicare typically covers 80% of the cost, so you may have some out-of-pocket expenses.
Summary: Will Insurance Cover TMS Therapy?
Will insurance cover TMS therapy? Yes, many insurance providers do cover TMS therapy, but there are specific requirements to qualify. You will likely need to show that you have tried other treatments without success and have a proper diagnosis from a healthcare professional. Costs can vary depending on your insurance plan, and if coverage is denied, there are still options to make TMS therapy accessible.
If you’re considering TMS therapy, talk to your healthcare provider and check with your insurance company to see if you qualify. Understanding your coverage options and preparing the necessary documentation can increase your chances of getting the treatment you need.
Get the Help You Need with TMS Therapy Coverage
Still, wondering if insurance will cover your TMS therapy? Contact American TMS Clinics today to discuss your options and eligibility. Our team is here to help guide you through the process, answer your questions, and ensure you get the treatment you deserve.